Top Performance
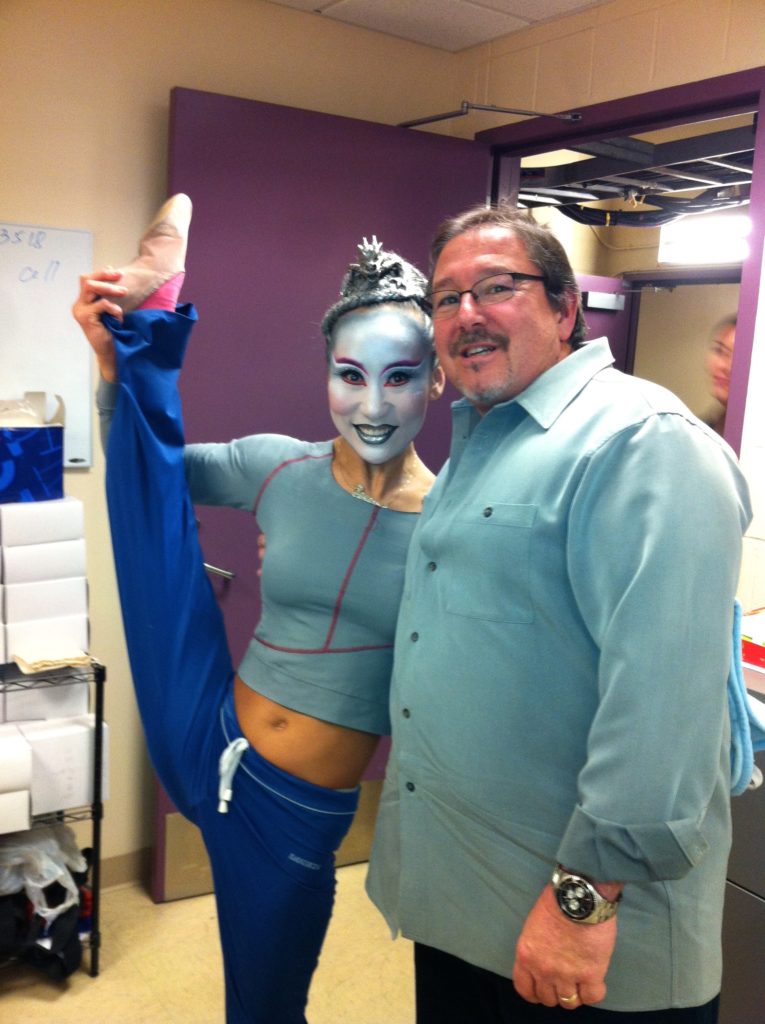
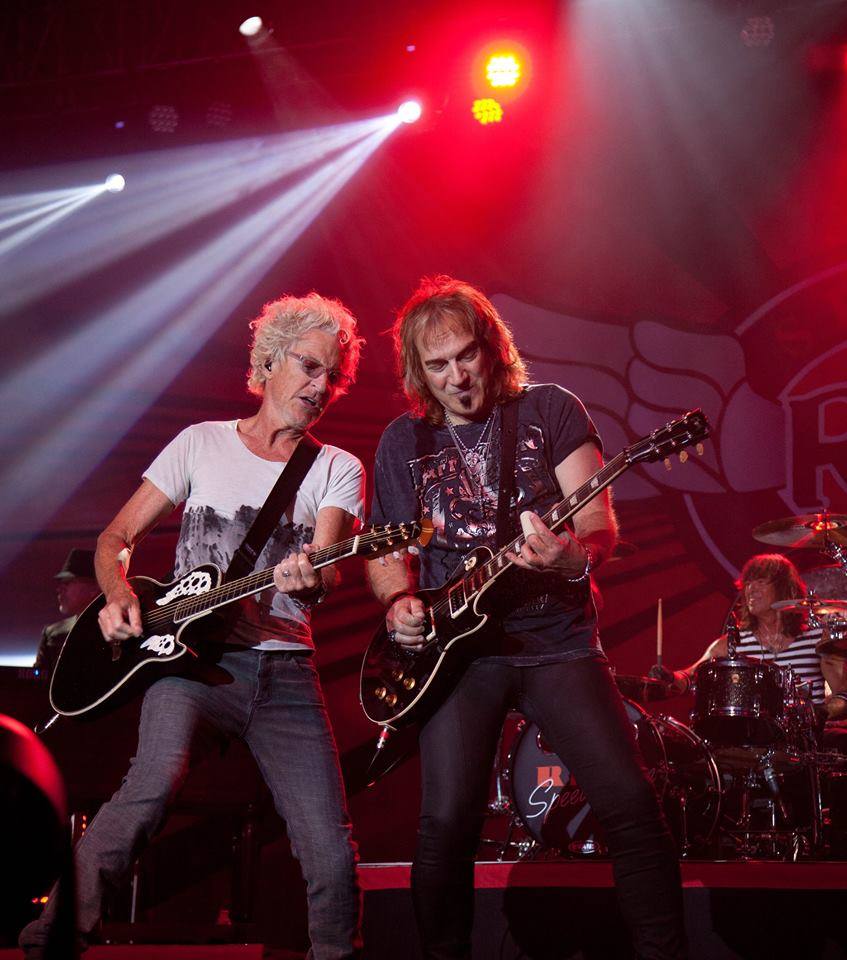
Dr. Luga Podesta has had over three decades of experience treating professional musicians, dancers and other performing artists with a proven track record keeping the best of the best on stage performing safely. For over 12 years, Dr. Podesta has written a monthly article titled the Rhythmic Physician DRUM! Magazine, contributing articles on health-related topics afflicting drummers and percussionists. As a sports medicine physician and musician, himself, he has a thorough understanding of the functional and biomechanical demands necessary for musicians and dancers to rehearse and perform day after day and night after night, regardless if you are drummer or percussionist, guitar player or keyboardist, a horn player or dancer. Dr. Podesta served as the Performance Medicine consultant for the Los Angeles based Cirque du Soleil show IRIS – A Journey through the World of Cinema, throughout the show’s creation and three-year existence in Los Angeles. Doctor Podesta continues to serve as the personal physician and consultant for many of the music industry’s most iconic musicians and bands.
Common Performing Arts Injuries
Although traumatic injuries can occur in musicians and performing artists, many of the injuries or conditions that performers sustain are secondary to repetitive stress, tissue overload and overuse. Whether you’re a violinist or a drummer, to develop the competency level required to excel, long hours of repetitive movement and practice is necessary. Dr. Podesta has extensive experience treating muscle, tendon, ligament, cartilage, bone and joint related traumatic, repetitive stress and overuse injuries in musicians and performing artists including:
Shoulder Pain
- Bursitis
- Labral tears
- Biceps, rotator cuff tendinitis
Elbow Pain
- Common flexor tendon (Golfers Elbow)
- Common extensor tendon (Tennis Elbow)
- Cubital tunnel syndrome (Ulnar Nerve)
Hand/Wrist Pain
- Carpal tunnel syndrome
- de Quervain’s tendonitis
- Trigger finger
- Triangular fibrocartilage complex (TFCC) tears
- Thumb UCL sprain
- Basal joint/thumb CMC arthritis
Hip Pain
- Arthritis
- Gluteal tendinitis
Knee Pain
- Patella tendinitis
- Quadriceps and Hamstring tendinitis
- Calf muscle strains
Ankle/Foot Pain
- Ankle sprains
- Achilles tendinitis
- Posterior tibialis and Peroneal tendinitis
- Plantar fasciitis
- Bunions
- Hallux rigidus
Neck & Low Back Pain
- Disc herniations
- Arthritis
- Nerve compression (pinched nerves)
When does neck pain become concerning?
Most causes of neck pain will eventually resolve in a short period of time. However, if your pain is not improving, has been present for 4 or more weeks, is worsening or associated with any of the below symptoms, medical evaluation is recommended.
- Electric shock like pain radiating down your arm or behind the
- Inability to stand
- Worsening pain with movement of the neck
- Worsening numbness and or tingling in your arms or hands
- Night pain
When does low back pain become concerning?
Most causes of low back pain will eventually resolve in a short period of time. However, if your pain is not improving, has been present for 4 or more weeks, is worsening or associated with any of the below symptoms, medical evaluation is recommended.
- Electric shock like pain radiating straight down from your low back to your foot
- Inability to stand
- Worsening pain with sitting or lying down
- Worsening numbness and or tingling in your lower extremities
- Pain with walking
- Tearing or ripping sensation in abdomen or low back
When low back pain is associated with these “Red Flags”:
- Bilateral sciatic pain (electric shock like pain running down the back of your leg)
- Bowel or Bladder dysfunction (especially urinary retention)-may indicate Cauda Equina Syndrome
- Sexual dysfunction-may indicate Cauda Equina Syndrome
- Night pain awakening you from sleep associated with unexplained weight loss- may indicate a malignancy
- Failure of bed rest to relieve pain-may indicate underlying systemic disease
- Associated with a febrile illness- may indicate underlying systemic infection, focal disk space infection or osteomyelitis
If any of the above mentioned “Red Flags” are present, medical attention should be sought immediately!
What is the difference between diagnostic versus therapeutic spinal injections?
A precision diagnostic spinal injection can help diagnose the precise cause of neck and low back pain, resulting in pain relief that occurs immediately after the procedure is completed. However, the local anesthetic by itself is not expected to provide long-term pain relief. When the exact cause of the spinal pain has been determined by the diagnostic injection, a variety of therapeutic injections can then be performed at the precise location indicated by the diagnostic injection.
What types of therapeutic spinal injections are indicated for neck and low back pain?
When cervical or lumbar spinal pain is not resolving on its own or is not responding to conservative spinal interventions such as oral medication, the application of therapeutic modalities such as ice or heat or physical therapy, it may become to necessary consider therapeutic spinal injections. Once a precision diagnostic spinal injection has localized the cause of pain, specific therapeutic injection therapies can then be utilized to target the various areas of the spine to provide a longer lasting therapeutic effect. Examples of some of these image (ultrasound of fluoroscopy) guided spinal injections utilizing corticosteroid and anesthetic medications, radiofrequency nerve ablations, and regenerative orthopedic therapies such as platelet rich plasma or progenitor cell-based injections. Some examples of the therapeutic injections that Dr. Podesta routinely performs include:
- Epidural and Caudal Injections: An epidural or caudal injection, places an anti-inflammatory steroid medication into the epidural space to decrease nerve root inflammation, to reduce pain in the low back and legs. By reducing inflammation, epidural injections help to promote healing an extended period of time.
- Cervical and Lumbar Facet Joint and Medial Branch/Dorsal Ramus Blocks: Not all spine pain emanates from the intravertebral disc or nerve roots. Facet joint pain is extremely common. Facet joint sensation including pain is transmitted from these joint to the brain by the median branch and dorsal ramus nerves. Blocking the transmission of pain signal from the facet joint to the brain with a short acting anesthetic, is extremely important diagnostic tool allowing us to precisely determine the exact location of the pain. Diagnostic median nerve and dorsal ramus blocks may be suggested when there is strong evidence to suspect the source of your pain is your facet joints.
- Radiofrequency Ablations: A radiofrequency ablation is a therapeutic procedure that uses an electrically generated radiofrequency current to generate heat that this disrupts the pain fibers of the median nerve and dorsal ramus that supplying sensation to the facet and sacroiliac joint. It is routinely performed to provide long-term relief for axial low back pain.
- Sacroiliac Joint Injections: The sacroiliac (SI) joints connect the lower spine (sacrum) with the pelvis (ilium). They transfer ground reaction forces from the lower leg and hip through the pelvis to the lumbar spine. Typically, these joints are very stable. However, the SI joints can move and undergo stress after restricted motion develops in the lumbar spine and hip. Image guided diagnostic SI joint injections with local anesthetic agents are used to determine if the joint is causing pain. The addition of a steroid medication or regenerative therapies such as PRP to diminish inflammation, a therapeutic effect can be provided.
- Lumbar Intervertebral Disc Injections: The intervertebral discs throughout the spine function to separate the vertebral bodies and exiting nerve roots. Disks can become painful when the lining of the disc known as the annulus tears and the nucleus, gel like structure within the disc leaks. Regenerative orthopedic procedures such as platelet rich plasma (PRP) and progenitor cell-based therapy with bone marrow concentrate (BMC) have proven beneficial in sealing, healing annulus tears and decreasing inflammation in and surrounding damaged discs.
These injections have been designed and are used clinically to diminish pain, improve function and prevent unnecessary spinal surgeries.
Can cell based therapies with PRP or progenitor cell-based treatments help?
Cell-based spinal therapeutic injections with platelet rich plasma (PRP) and progenitor cell (stem cell) therapies provide state of the art treatments for acute and degenerative spinal conditions which have the potential to stimulate the immune system and increase the body’s natural ability to heal damaged tissues such as intervertebral discs, diminish inflammation or facet joints, stabilize supporting spinal ligaments resulting in overall pain reduction and functional improvement. Cell-based therapies can provide patients with low back pain from a variety of causes with long-term relief from pain improving mobility and function with faster recovery times. Cell-based therapeutic spinal therapies can significantly reduce time away from family, sports, work or daily activities while delaying or completely avoiding the need for surgery and prescription medication.
Tendon Injuries
Tendonitis:
 Tendinitis is an acute inflammatory condition affecting tendons typically where they attach on a bone. It is described by several names including tennis elbow, golfers’ elbow, jumpers’ knee or swimmers’ shoulder. Regardless of the name, tendinitis can be painful, debilitating and effect any tendon. Early treatment is extremely important to minimize the long-term risks and effects of tendon injury. Dr. Luga Podesta has both the experience, knowledge, and skill to minimize those risks. Dr. Podesta is a regenerative orthopedic and sports medicine expert with over 3 decades of experience who can offer cutting edge regenerative medicine and orthopedic treatments to stimulate and enhance tendon healing to improve your body’s natural healing capacity.
Tendinitis is an acute inflammatory condition affecting tendons typically where they attach on a bone. It is described by several names including tennis elbow, golfers’ elbow, jumpers’ knee or swimmers’ shoulder. Regardless of the name, tendinitis can be painful, debilitating and effect any tendon. Early treatment is extremely important to minimize the long-term risks and effects of tendon injury. Dr. Luga Podesta has both the experience, knowledge, and skill to minimize those risks. Dr. Podesta is a regenerative orthopedic and sports medicine expert with over 3 decades of experience who can offer cutting edge regenerative medicine and orthopedic treatments to stimulate and enhance tendon healing to improve your body’s natural healing capacity.
Tendinitis is an inflammatory process effecting tendon where it attaches to a bone. A tendon is a cord light fibrous tissue the functions to attach a muscle to a bone to provide movement of a joint. Tendinitis occurs due to an acute injury or commonly is the result of a sports injury or repetitive activities and movement from a job or other activity. The most common parts of the body affected by tendinitis include:
- Shoulder – Biceps, rotator cuff tendons
- Elbow – Common flexor tendon (Golfers elbow); Common extensor tendon (Tennis elbow)
- Hip – Gluteal tendons (Medius and Minimus Tendons)
- Knee – Patella tendon, Quadriceps tendon, Hamstring and gastrocnemius tendons.
- Ankle – Achilles, posterior tibialis tendons, peroneal tendons
- Foot – Achilles tendon, plantar fascia
How are tendons treated?
The initial inflammatory phases of tendinitis are typically short lived and responsive to conservative treatment including rest, oral NSAID medications, therapeutic modalities such as ice and heat, physical therapy, and activity modification. However, when longer lasting, chronic or after tendinosis develops, more aggressive injection therapies or regenerative orthopedic procedures are required such as:
- Corticosteroid Injection: Cortisone injections have been used to relieve pain and treat inflammatory conditions like tendonitis for years. These injections are most often performed in the physician’s office. Cortisone is typically combined with local anesthetic medication such as lidocaine or Marcaine. Due to potential side effects and systemic risks such as muscle, tendon and ligament weakening, articular cartilage damage, bone death (avascular necrosis), nerve damage, infection and elevation of blood sugar in diabetics; the number of injections you can receive in a year are limited.
- Platelet Rich Plasma (PRP) Treatments: Platelet rich plasma therapy has become the treatment of choice for early tendonitis. PRP, is performed to stimulate and further enhance our natural healing response when injected in an injury by concentrating growth factor containing platelets and circulating progenitor cells in plasma ultimately reducing pain and increasing tendon function by decreasing inflammation, stimulating tendon healing and functional improvement.
- Progenitor cell (Bone Marrow Concentrate) Treatment: Previously referred to as “Stem Cell Therapy”, progenitor cell-based treatments are reserved for more severe tendon conditions such as tendinosis, calcific tendinosis or partial tendon tears. Collecting small amount of bone marrow from the patient. The marrow is concentrated and reinjecting back into the injury site or abnormal joint. Bone marrow concentrate in addition to PRP has shown promise to further diminish inflammation, promote and stimulate normal tendon growth not observed with PRP alone. Progenitor cell-based therapy is performed in regenerative orthopedics to enhance the body’s natural healing mechanisms and capabilities to treat orthopedic conditions involving tendons throughout the body.
- Autologous Conditioned Serum: Autologous conditioned serum is performed by drawing a small sample of a patient’s own blood, allowed to remain in a clotted for at body temperature for 3 to 4 hours, centrifuged to separate the clot from its serum. The serum, which contains increased levels of autologous interleukin one receptor antagonist is the injected back into the injured joint or tissue within 6 hours of the initial blood draw. IL1RA has been used in Europe since 2003 under the names Orthokine and Regenokine, is currently under investigation for the treatment of inflammatory conditions involving tendons, ligaments and joints as a more physiologically natural and safer alternative to corticosteroids.
- Alpha 2 macroglobulin Injection (A2M): Alpha 2 macroglobulin is another regenerative orthopedic therapy being used more frequently to treat osteoarthritis. A2M provides joint preservation qualities when injected into a damaged joint higher at concentrations to target destructive enzymes. It is felt to help promote natural healing, tissue growth and prevent articular cartilage breakdown.
- Amniotic Fluid Allographs: Amniotic tissue and amniotic membrane is a protective barrier in the human placenta. It is typically discarded after a baby is delivered. There is scientific evidence that the fluid derived from processing amniotic tissue is a source of biologic proteins, growth factors and progenitor cells. Placental tissue is donated after cesarean birth and processed. The fluid obtained after the processing, has been shown to exhibit a variable cellular, growth factor and biologic protein content, which can significantly affect regenerative quality. Studies have observed there are no live progenitor cells present in preserved amniotic fluid allographs. The use of amniotic fluid allografts has been restricted in patients who were unable to use their own natural cells due to chronic illness, medication use, history of recent or active treatment of a malignancy, chemo or radiation therapy.
If you have been experiencing pain from a tendon that hasn’t improved, don’t wait until it’s too late. Dr. Luga Podesta can quickly determine the cause of your pain and provide the cutting edge regenerative orthopedic therapy necessary to get back in the game.
Ligament Injuries
What is the difference between a sprain and a strain?
Sprains and strains are injuries that occur in soft tissue, however, the difference between sprains and strains lies within the tissue that they occur. Sprains occur in ligaments, whereas strains occur in muscles and tendons.
How are ligament injuries diagnosed?
Making a diagnosis of a ligament injury requires taking a detailed history describing the mechanism of injury location of pain and circumstances associate at the time of injury, hearing or feeling a pop for a tearing sensation in a particular joint. Performing a thorough dynamic joint stability exam with comparison to the non-injured side can be helpful when a ligament injury is suspected. Imaging studies such as stress x-rays, MRI scans or dynamic ultrasound valuations are important to detect any radiographic abnormalities as well as abnormalities specifically within a particular ligament with a suspected injury.
How are ligament injuries treated non-surgically?
The initial inflammatory phases are typically short lived and responsive to conservative treatment including the R.I.C.E. treatment principles plus: relative rest, oral NSAID medications, therapeutic physical modalities such as ice and heat, bracing to maintain stability and compression, elevation, protected movement and activity modification. However, for injuries that don’t respond to conservative treatments or with more severe cases when joint stabilization is priority, regenerative orthopedic injection procedures may be helpful to prevent the need for surgical stabilization procedures, prolonged recovery periods and delayed return to sports and normal function.:
- Platelet Rich Plasma (PRP) Treatments: Research has proven that Platelet rich plasma therapy can be a helpful treatment for mild and moderate ligament injuries. PRP, is performed to stimulate and further enhance our natural healing response when injected in an injury by concentrating growth factor containing platelets and circulating progenitor cells in plasma ultimately reducing pain and increasing tendon function by decreasing inflammation, stimulating ligament healing and functional improvement.
- Bone Marrow Concentrate (Progenitor cell) Treatment: Previously referred to as “Stem Cell Therapy”, progenitor cell-based treatments are reserved for more severe ligament conditions such as higher-grade acute sprains, chronic degenerative sprains or partial ligament tears. Collecting small amount of bone marrow from the patient. The marrow is concentrated and reinjecting back into the injury site or abnormal joint. Bone marrow concentrate in addition to PRP has shown promise to further diminish inflammation, promote and stimulate ligament growth not observed with PRP alone. Progenitor cell-based therapy is performed in regenerative orthopedics to enhance the body’s natural healing mechanisms and capabilities to treat orthopedic conditions involving tendons throughout the body.
- Amniotic Fluid Allographs: Amniotic tissue and amniotic membrane is a protective barrier in the human placenta. It is typically discarded after a baby is delivered. There is scientific evidence that the fluid derived from processing amniotic tissue is a source of biologic proteins, growth factors and progenitor cells. Placental tissue is donated after cesarean birth and processed. The fluid obtained after the processing, has been shown to exhibit a variable cellular, growth factor and biologic protein content, which can significantly affect regenerative quality. Studies have observed there are no live progenitor cells present in preserved amniotic fluid allographs. The use of amniotic fluid allografts has been restricted in patients who were unable to use their own natural cells due to chronic illness, medication use, history of recent or active treatment of a malignancy, chemo or radiation therapy.
If you have been experiencing pain from a ligament sprain that hasn’t improved, don’t wait until it’s too late. Dr. Luga Podesta can quickly determine the cause of your pain and provide the cutting edge regenerative orthopedic therapy necessary to get back in the game.
Arthritis
How is arthritis diagnosed?
Dr. Podesta can you confirm the diagnosis of arthritis after completing a thorough history and physical exam and imaging studies such as X-rays and possibly MRI. If a rheumatologic or infectious process suspected specific laboratory blood tests and joint fluid analysis maybe necessary to confirm diagnosis the specific cause.
What treatments are available for arthritis?
Treatment of arthritis is dependent on the stage of arthritis and the severity of symptoms. For mild arthritis with minimal symptoms, activity modification is often recommended and adequate to relieve mild symptoms. However, for more advanced cases with more severe symptoms, multiple nonsurgical and minimally invasive regenerative orthopedic treatments are available to maximize our bodies natural ability to repair and heal, ultimately relieving pain and improving function. Dr. Luga Podesta can determine the precise regenerative orthopedic therapy or combination of therapies that are best for you, including:
- Corticosteroid Injection: Cortisone injections have been used to relieve pain and treat inflammation conditions for years. These injections are most often performed in the physician’s office. These injections have been believed to be most effective in treating inflammatory arthritis, like rheumatoid arthritis. Cortisone is typically combined with local anesthetic medication such as lidocaine or Marcaine. Due to potential side effects and systemic risks such as articular cartilage damage, bone death (avascular necrosis), nerve damage, infection, elevation of blood sugar in diabetics, muscle tendon and ligament weakening; the number of injections you can receive in a year are limited.
- Viscosupplementation Injections: This is an injection or series of injections of a hyaluronan (hyaluronic acid) preparation into a joint for the treatment of arthritis. Hyaluronic acid is a natural substance in our joint fluid that assists in joint lubrication. It helps to provide a friction free surface allowing smooth movement of the articular cartilage covering the joint. Viscosupplementation injections can provide symptomatic pain relief while delaying the need for surgery.
- Platelet Rich Plasma (PRP) Treatments: Platelet rich plasma therapy is performed to stimulate and further enhance our natural healing response when injected in an injury by concentrating growth factor containing platelets and circulating progenitor cells in plasma ultimately providing a joint preservation affect by decreasing inflammation, reducing pain, stimulate healing and improve joint function.
- Progenitor cell (Bone Marrow Concentrate) Treatment: Previously referred to as “Stem Cell Therapy”, progenitor cell-based treatments begin by collecting small amount of bone marrow from the patient. The marrow is concentrated and reinjecting back into the injury site or abnormal joint. It is used to diminish inflammation, promote healing of articular cartilage and soft tissue such as meniscus, periarticular capsule, supporting ligaments and stimulate bone growth. It assists to reestablish a normal intraarticular environment, slow the degenerative process and help preserve the natural joint. Progenitor cell-based therapy is performed in regenerative orthopedics to enhance the body’s natural healing mechanisms and capabilities to treat a variety of orthopedic conditions involving joint and soft tissue.
- Interosseous Bioplasty Injection (IOBP): This is a regenerative orthopedic treatment that targets bone pathologies resulting from acute or chronic injury including osteoarthritis, persistent bone bruises, insufficiency fractions or avascular necrosis. The procedure is performed to stimulate physiologic subchondral bone remodeling, healing and involves delivering a combination of PRP, BMC and autologous thrombin into the injured bone. The treated bone is then protected over a 4-6 week period to optimize healing potential.
- Autologous Conditioned Serum: Autologous conditioned serum is performed by drawing a small sample of a patient’s own blood, allowed to remain in a clotted for at body temperature for 3 to 4 hours, centrifuged to separate the clot from its serum. The serum, which contains increased levels of autologous interleukin one receptor antagonist (IL1RA) is the injected back into the injured joint or tissue within 6 hours of the initial blood draw. IL1RA has been used in Europe since 2003 under the names Orthokine and Regenokine, is currently under investigation for the treatment of inflammatory conditions as a more natural and safer alternative to corticosteroids.
- Alpha 2 macroglobulin Injection (A2M): Alpha 2 macroglobulin is another regenerative orthopedic therapy being used more frequently to treat osteoarthritis. A2M provides joint preservation qualities when injected into a damaged joint higher at concentrations to target destructive enzymes. It is felt to help promote natural healing, tissue growth and prevent articular cartilage breakdown.
- Amniotic Fluid Allographs: Amniotic tissue and amniotic membrane is a protective barrier in the human placenta. It is typically discarded after a baby is delivered. There is scientific evidence that the fluid derived from processing amniotic tissue is a source of biologic proteins, growth factors and progenitor cells. Placental tissue is donated after cesarean birth and processed. The fluid obtained after the processing, has been shown to exhibit a variable cellular, growth factor and biologic protein content, which can significantly affect regenerative quality. Studies have observed there are no live progenitor cells present in preserved amniotic fluid allographs. The use of amniotic fluid allografts has been restricted in patients who were unable to use their own natural cells due to chronic illness, medication use, history of recent or active treatment of a malignancy, chemo or radiation therapy.
An expert in analyzing, diagnosing and treating injuries sustained by all musicians and dancers including drummers, percussionists, guitarists, keyboard players, dancers and other performing artists. Dr. Podesta has a proven track record for keeping the “Best of the Best” on stage performing safely and at their highest ability by providing a cutting-edge comprehensive non-surgical approach, evaluation and holistic treatment recommendations, advanced regenerative orthopedic treatments to stimulate and enhance your body’s natural healing capacity. You don’t need to be a Pro to be treated like one.

